Key Points:
- Nicotinic acid has a long history of being used to lower “bad” LDL cholesterol, but has fallen out of favor with the advent of statins.
- Combining nicotinic acid with the longevity-associated compounds berberine and quercetin, along with tocotrienols, which are related to vitamin E, lowers LDL cholesterol and fats while dramatically increasing “good” HDL cholesterol.
Modern medicine has led many to perceive expensive prescription medications as the most viable remedies for treating age-related conditions like high cholesterol. However, not all doctors are apt to push lipid-lowering medications like statins, knowing of their potential side effects. Namely, Joseph Keenan, MD, Professor Emeritus at the University of Minnesota, points out that statin use is associated with an increased risk of dementia. Moreover, in The Niacin Rebirth, Dr. Keenan explains why niacin is a great scientifically-backed alternative to statins.

A Changing World Necessitates a New Approach
It’s been plain to see that regular aerobic exercise and consuming fewer calories, particularly in the form of saturated fats and refined sugars, leads to lower LDL cholesterol and improved cardiovascular outcomes. Still, notwithstanding efforts to promote healthy habits, cardiovascular disease remains the leading cause of death worldwide. Furthermore, as the world population grows, it will grow older, and the number of individuals over the age of 65 is expected to increase dramatically within the next few decades.
As the number of older individuals increases, so too will the prevalence of age-related chronic conditions like cancer, dementia, and cardiovascular disease. Some predict that this explosion of disease will strain the healthcare systems of national governments, potentially compromising economic growth and stability. Dr. Keenan argues that the global increase in disease burden requires a paradigm shift in how we care for older adults. Such a paradigm shift, says Dr. Keenan, could benefit from exploring a return to nicotinic acid as an anti-aging therapy.
A Short History of Nicotinic Acid’s Effects
Nicotinic acid (NA) is not anything new. Also called vitamin B3, NA occurs naturally in the body and is essential for survival. NA caught the attention of scientists in the early 1900s, when vitamin B3 deficiency was found to cause pellagra. It was in response to a pellagra outbreak, afflicting mostly malnourished farmers in the United States, that scientists began to synthesize niacin, which today is synonymous with vitamin B3 and NA. It wasn’t until 1955 that scientists discovered that NA lowers cholesterol in human subjects.

Improves Lipid (Fat & Cholesterol) Levels and Reduces Heart Disease Risks
Over the next 50 years, NA was established as a broad-spectrum lipid-modulating drug that increases HDL cholesterol by up to 35% while decreasing triglycerides (fats) by up to 50% and LDL cholesterol by up to 15%. It was one of the first compounds shown to reduce the risk of heart attacks, also lowering the risk of mortality by 11% in The Coronary Drug Project (1966-1975). Subsequent studies have supported these initial findings, showing that NA reduces the risk of adverse cardiovascular events. For example, in a 2019 analysis of 17 human trials, NA was shown to reduce the risk of stroke and other lethal cardiovascular events.
Lowers Inflammation
In addition to improving lipid levels, NA reduces inflammation, which is a key contributor to the development of heart disease. In 2024, an analysis of 15 human trials showed that NA administration significantly reduced the inflammatory markers CRP (C-reactive protein) and TNF-⍺. Evidence demonstrates that the anti-inflammatory effects of NA are independent of its lipid-lowering effects and mediated by an NA receptor called GPR109A, which is expressed on immune cells. Therefore, NA is both a lipid-lowering and anti-inflammatory compound.
Lowers Precise Predictors of Heart Disease
“NA is the only agent that can improve every form of dyslipidemia, making it the best agent with which to initiate treatment of dyslipidemia in all persons, especially older persons,” according to Dr. Keenan in The Niacin Rebirth.
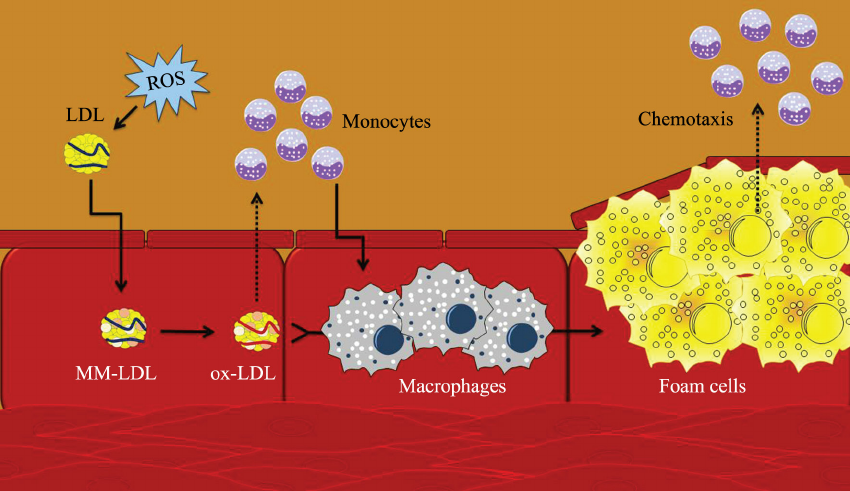
Keenan points out that NA reduces the oxidized form of LDL cholesterol. It is the oxidized form that leads to the buildup of plaques in the arteries, a condition known as atherosclerosis, the most common form of heart disease. In middle-aged adults, dietary NA intake was associated with lower levels of oxidized LDL cholesterol. The oxidation of LDL cholesterol can occur in response to oxidative stress, an underlying biological driver of aging. NA was shown to significantly reduce oxidative stress in patients with high cholesterol.
Similar to oxidized LDL cholesterol, Lp(a) is a more precise predictor of atherosclerosis than total LDL cholesterol. Like LDL (low-density lipoprotein) and HDL (high-density lipoprotein), Lp(a) [lipoprotein (a)] is a lipoprotein—a particle composed of lipids and proteins that carries lipids through the bloodstream. Lp(a) contains a protein called apolipoprotein(a), which is what differentiates it from LDL, and makes it more likely to form artery plaques.
An analysis of 17 human trials showed that NA treatment is associated with a significant reduction in Lp(a) levels. In contrast, statins have been shown to increase Lp(a) levels by 20%. It’s important to reiterate that high LDL cholesterol is only a marker of atherosclerosis, and Lp(a) is a better marker. With that being said, an analysis of 11 human trials showed that NA reverses the progression of atherosclerosis.
How Statins Stomped Nicotinic Acid’s Potential
In The Niacin Rebirth, Dr. Keenan explains that the success of NA in The Coronary Drug Project was tarnished due to participants dropping out of the study because of an irritating side effect: flushing of the skin. The focus of NA research then shifted to extended-release versions of NA, which reduce or eliminate the flushing side effect. However, by this time, in the 1990s, the first statin had earned approval from the FDA (Food and Drug Administration). This was followed by two large studies that further tarnished the reputation of NA as a viable cholesterol-lowering compound.
Aim High and Thrive
In the AIM-HIGH (Atherothrombosis Intervention in Metabolic Syndrome with low HDL/High Triglycerides: Impact on Global Health Outcomes) trial, participants were given a combination of NA and a statin called simvastatin. Keenan explains that the trial was stopped prematurely, after three years instead of seven years, because the researchers suspected that NA/simvastatin would increase the incidence of stroke. This was later found to be a statistical error, but it was already too late, as scientists, physicians, and the masses now perceived NA as inferior or even harmful relative to statins.

Keenan also highlights another study with a ridiculously long name called the HPS2-THRIVE (Heart Protection Study 2: Treatment of HDL to Reduce the Incidence of Vascular Events) trial. The participants of this study were already taking statins and given NA and an anti-inflammatory drug called laropiprant to reduce flushing. In this global study, it was found that statins/NA/laropiprant increased the risk of adverse conditions like diabetes and muscle disease, particularly in Chinese participants. Keenan alludes to these adverse events being triggered by laropiprant, attributing the results to poor study design.
Keenan also mentions that NA treatment should last at least six years before seeing cardiovascular benefits. The AIM-HIGH and HPS2-THRIVE trials both lasted for less than four years. Moreover, in these large studies with ties to pharmaceutical companies like Merck & Co., NA was always administered with statins. The effects of NA were not tested alone. Thus, many institutions conclude that NA provides no additional benefits to statin administration, yet there have been no studies that have compared the cardiovascular outcomes of NA to those of statins alone.
Nicotinic Acid Combo Reduces Lipid Levels
In a study conducted by Dr. Keenan, ten older adults were given a combination of extended-release compounds:
- NA: A lipid-lowering, anti-inflammatory compound that also boosts NAD+ levels.
- Dihydroberberine: A highly bioavailable form of berberine, associated with combating age-related diseases like type 2 diabetes.
- Toxifolin (dihydroquercetin): A form of quercetin, a polyphenol and senolytic (compound that eliminates age-promoting senescent cells).
- Mixed tocotrienols: Molecules related to vitamin E that act as powerful antioxidants.
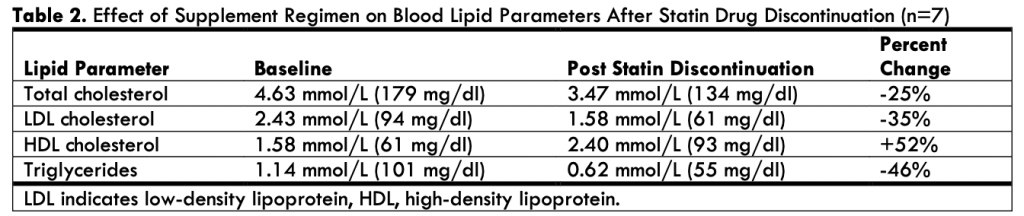
After 16 weeks, the seven participants who were taking statins were able to discontinue use. They exhibited a 25% reduction in total cholesterol, a 35% reduction in LDL cholesterol, a 46% reduction in triglycerides, and a 52% increase in HDL cholesterol. Some participants experienced flushing, upset stomach, or liver damage, as determined by high AST (aspartate aminotransferase) and ALT (alanine aminotransferase) levels. The patients with liver damage were told to go off NA until AST and ALT levels went back to normal and resume (lower) maintenance doses. Aspirin was given to participants to reduce flushing.
Study Limitations
Firstly, the study was small and did not include a placebo group, so it is difficult to determine whether the lipid levels of the participants would have decreased otherwise (including from taking statins), had they not taken the NA stack. Secondly, the participants were told to exercise regularly, which could have accounted for the improved lipid levels. However, exercise was not quantified or correlated with any of the measurements. Thirdly, it is difficult to determine which of the compounds in the combination stack was most responsible for the lipid-lowering effects.
Taking Nicotinic Acid to Slow Aging
It seems clear that NA is capable of improving lipid levels, particularly in individuals at risk for heart disease, such as those with high LDL cholesterol levels. While statins may lower LDL cholesterol more than NA, NA lowers more precise markers of heart disease, including oxidized LDL cholesterol and Lp (a). After taking into account the side effects of each compound, it is difficult to assess which compound is better for slowing cardiovascular aging, as they have not been compared directly. The perception is that statins are superior to most other compounds when it comes to reducing the risk of cardiovascular-related death, but this may not be the case.