- Stem Cells Have the Capacity to Develop into Multiple Tissue Cell Types
- Seven Stem Cell Subtypes Countering Different Age-Related Conditions
- Adult Stem Cells Are Easier to Obtain
- Stem Cells’ Therapeutic Effects Come from Vesicle Signaling
The World Health Organization estimates that the global population over age 60 will reach 2 billion by 2050. With the accelerating growth of the world’s aging population, finding ways to counter aging’s adverse health effects has become paramount to extending the number of years people live without disease (healthspan).
An intriguing way to fight the ravages of aging, stem cell therapy, has received increasing attention in the last 40 years or so. The usage of stem cells for health research entered the limelight in 1981. At that time, scientists isolated embryonic stem cells derived from cell clusters from fertilized mouse embryos — blastocysts. Moreover, in 1999, Science named stem cell research at the very top of the 10 most important research fields in the 21st century. As such, taking a closer look at stem cell therapy’s effects against age-related conditions and where this research field is heading is necessary to understand its importance in aging research.
Research has shown that seven different types of stem cells — embryonic, induced pluripotent, neural, bone marrow, dental pulp, adipose-derived, and umbilical cord stem cells — can develop into tissues like cartilage, bone, and muscle to alleviate age-associated diseases. Evidence from stem cell therapy research supports that stem cells’ anti-aging benefits result from their ability to relay cell signals via exosomes – vesicles carrying molecular signaling cargo – to nearby cells.
Stem Cells Have the Capacity to Develop into Multiple Tissue Cell Types
All stem cells are undifferentiated, meaning that they haven’t transformed into a specific cell type for integration into tissue. Stem cells have self-renewal abilities and the potential to differentiate into multiple types of cells. Along those lines, stem cells have the ability to regenerate various cells, tissues, and organs.
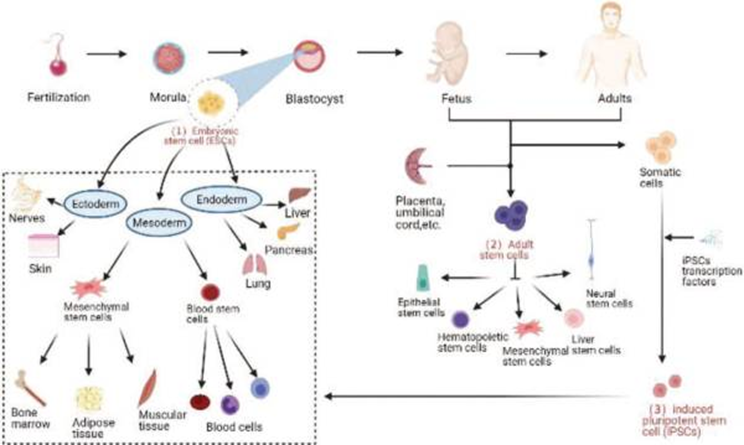
There are three classes of stem cells: embryonic stem cells, adult stem cells, and induced pluripotent stem cells (iPSCs). Embryonic stem cells, derived from fertilized embryos, are distinguished from adult stem cells by their developmental stage. Embryonic stem cells have a high capacity to replicate and transform – differentiate – into any type of cell in the body (totipotency), form tissues and organs, and eventually develop into a complete individual. Adult stem cells, on the other hand, can be isolated from various tissues and organs, such as bone marrow, fat tissue (adipose tissue), umbilical cord blood, and the placenta. Compared to embryonic stem cells, adult stem cells have the potential to differentiate into a lower range of cell types in the body, from several cell types (pluripotency) to only one (unipotency), depending on the type of adult stem cell.
The third type of stem cell, iPSCs, were added to the repertoire of stem cells with their discovery in 2006. iPSCs are a type of cell that forms the structural framework of animal skin (fibroblasts) that are transformed into a pluripotent state by stimulating four genes within them – Oct4, Sox2, Klf4, and c-Myc. As pluripotent stem cells, iPSCs have the potential to differentiate into a wide array of cell types and are used for anti-aging procedures like cell replacement as well as having rejuvenating effects on nearby cells.
Seven Stem Cell Subtypes Countering Different Age-Related Conditions
As pluripotent cells, embryonic stem cells have the ability to differentiate into any type of cell in the body. Scientists isolate this type of stem cell from cell clusters derived from fertilized embryos – blastocysts – in laboratory dishes (in vitro).
Researchers have studied embryonic stem cell therapy in humans and animal models, including mice and rats. Embryonic stem cell injections into mice with poor ovarian function improved ovarian function. A human study also showed that embryonic stem cells improved heart function following heart tissue injury (ischemia/reperfusion injury).
Theoretically, embryonic stem cells are a promising strategy to fight age-related diseases; however, the usage of this cell type is limited by ethical concerns. Since the isolation of embryonic stem cells requires the use of an aborted embryo, states have limited the use and development of this therapeutic technique.
iPSCs were discovered in 2006 when Yamanaka and Takahashi reprogrammed mouse fibroblasts to a pluripotent state with proteins called Yamanaka factors, which stimulate four genes (Oct4, Sox2, Klf4, and c-Myc). According to Science, who ranked iPSCs as one of the top 10 scientific and technological advancements in the world, the development of iPSCs represents a turning point in stem cell therapy.
In 2007, researchers in the United States and Japan reported the successful induction of human fibroblasts to iPSCs. Mouse studies using iPSCs have achieved promising results in the treatment of skin defects, diabetes, and gut inflammation (enteritis).
iPSCs use patients’ own cells, thereby avoiding immune rejection issues. iPSC technology is still in its beginning stages; however, many scientists believe that future iPSC research will result in the wide use of these stem cells for clinical disease treatment.
Adult Stem Cells Are Easier to Obtain
Compared to embryonic stem cells and iPSCs, adult stem cells have limited differentiability, meaning that they can only differentiate into a limited number of tissue types, depending on the tissue from which they originate. Adult stem cells are easy to obtain, though, making their use in medical research and clinical treatment more feasible. Adult stem cells for therapeutic purposes include the subtypes of neural stem cells, bone marrow mesenchymal stem cells, umbilical cord mesenchymal stem cells, adipose-derived mesenchymal stem cells, and dental pulp stem cells.
Aging can wreak havoc on brain function and drives neurodegenerative disease with increasing prevalence due to the aging population. Most inherited age-associated neurodegenerative diseases have no cure; however, increasing evidence suggests that neural stem cells provide a promising tool to treat nervous system diseases. Neural stem cells can differentiate into multiple nervous system cell types, including neurons, astrocytes, and oligodendrocytes. As for treating presently incurable neurological diseases, Huang and colleagues have reported neural stem cell therapy successfully improving protein plaque (Aꞵ plaques) clearance in an Alzheimer’s disease mouse model. In the same study, neural stem cell therapy improved neuron survival and neural regeneration. In another study, Kim and colleagues isolated neural stem cells from a cluster of neurons grown in a laboratory dish and treated a Parkinson’s disease rat model with them. In doing so, the researchers successfully increased the number of neurons that decline in Parkinson’s disease, which play essential roles in motor movements – dopaminergic neurons. What’s more, treating a mouse model for stroke with neural stem cells gave physical function improvements and triggered the production of new neurons in the brain – neurogenesis. In humans, a completed clinical trial utilized neural stem cell injections in amyotrophic lateral sclerosis (ALS) patients and showed that neural stem cell therapy is safe and can help with deteriorating physical function in ALS. These studies provide evidence that this technique may be used successfully to combat aging-related neurological conditions.
Currently, no neural stem cell therapy has been approved for routine clinical treatment. Studies have demonstrated the safety of applying this technology, though. As such, new breakthrough research using neural stem cell therapy could provide ways to treat currently incurable neurological disorders like Parkinson’s disease and Alzheimer’s disease.
Bone marrow mesenchymal stem cells come from bone marrow and have the ability for self-renewal and differentiation into multiple types of cells. Interestingly, a number of animal studies suggest that bone marrow stem cells can be used to delay or reverse aging. For example, Zhou and colleagues injected bone marrow mesenchymal stem cells from young mice into older mice and found that the young mice bone marrow stem cells reversed signs of spleen aging. In humans, a clinical trial was completed showing that bone marrow mesenchymal stem cells were safe, well-tolerated, and feasible for the treatment of ALS. In this study, ALS symptoms such as physical functioning difficulties were improved. According to the U.S. Library of Medicine, most of the 759 studies registered for bone mesenchymal stem cells have been completed, and they show effectiveness in multiple diseases. The only drawback to using bone marrow mesenchymal stem cells is that their use may trigger an increased risk of tumor formation in some patients.
Another type of adult stem cell therapy gaining popularity is the use of umbilical cord mesenchymal stem cells, derived from umbilical cord blood or tissue surrounding the umbilical cord. Compared to other types of adult stem cells like bone marrow mesenchymal stem cells, umbilical cord mesenchymal stem cells have greater proliferative capabilities, making this type of stem cell therapy promising for future clinical usage.

Umbilical cord mesenchymal stem cells exert anti-aging effects by rejuvenating and repairing aging cells, tissue, and organs. A study of mice with premature ovarian failure, where ovaries cease to be functional at an early age, showed that umbilical cord mesenchymal stem cell therapy improved ovarian function. Moreover, in human COVID patients, umbilical cord mesenchymal stem cell therapy significantly increased the survival rate of these patients. Moreover, the same study showed that this form of stem cell therapy is safe. What’s more, a cumulative umbilical cord mesenchymal stem cell therapy article that pooled multiple studies together reveals that these stem cells can be safely used in the nervous system, cardiovascular system, kidney, immune system, liver, lung, and skin conditions. All of these findings make umbilical cord mesenchymal stem cells a promising cell type in the stem cell family.
Adipose-derived mesenchymal stem cells come from fat tissue and can differentiate into bone, muscle, cartilage, and fat tissue (adipose tissue). Adipose-derived mesenchymal stem cells are often used to regulate inflammation and promote wound healing. A mouse study found that therapy with these stem cells improved diabetes. In humans, patients with hair loss (alopecia) exhibited improved hairlines after adipose-derived mesenchymal stem cell therapy.
Adipose tissue and adipose-derived mesenchymal stem cells are abundant throughout the body, making the isolation of adipose-derived mesenchymal stem cells relatively easy. However, these cells’ proliferation in laboratory dishes is quite limited, which hinders their clinical application.
The last type of adult stem cell is the dental pulp stem cell, which can be derived from the central pulp cavity of each tooth. These stem cells can differentiate into tooth, cartilage, fat, and nerve-like cells. One study using this type of stem cell therapy focused on alleviating arthritis in the mouth of a mouse model with positive results. Research on dental pulp stem cells remains in exploratory phases, and many challenges remain.
Stem Cells’ Therapeutic Effects Come from Vesicle Signaling
A key question about how stem cells help fight age-related conditions in experiments with animal models and in human trials revolves around effects coming from stem cell replacement or signaling to nearby cells. Increasing evidence shows that stem cell-derived exosomes – vesicles released by stem cells that contain signaling molecules – confer stem cells’ rejuvenating effects like improved immunity and cell proliferation. With that in mind, some researchers are now studying injections of exosomes derived from stem cells to harness the benefits of stem cell therapy. Stem cell exosome injections come with reduced chances of adverse immunological responses and diminished odds of tumor formation, thereby improving treatment safety. Along those lines, stem cell exosomes and their therapeutic applications are currently the hottest topic in precision medicine. Therapeutic strategies that utilize stem cell exosomes are currently under development at an astonishing speed.