Key Points:
- Cell-free synthetic artificial stem cells (SASC) were developed to overcome problems associated with living stem cells.
- SASC reduces inflammation in a cell model for arthritis — a disease characterized by inflammation and degeneration of the joints.
- Degeneration and swelling of the knee joints are reduced by SASC in rats.
It was once thought that the magic of stem cells proceeded from their ability to repair organs by replacing damaged cells. However, while stem cells are capable of repairing damaged tissue, their integration into that tissue has been found to be almost non-existent. Now scientists postulate that it is the secretions of stem cells and not stem cells themselves that are responsible for tissue repair.
As reported in PNAS, researchers from the University of Connecticut have developed synthetic artificial stem cells (SASC), which eliminates the need for keeping cells alive and healthy. Shah and colleagues show that SASC can reduce inflammation in a cell model for arthritis. They also show that SASC can reduce joint degeneration and swelling in a rat model for arthritis. Since SASC are made of tiny plastic spheres, they are easier to store and maintain than living stem cells.
Plastic Stem Cells Reduce Cartilage Inflammation and Degeneration
Signaling molecules secreted by stem cells called growth factors are capable of promoting tissue regeneration and growth. Shah and colleagues loaded four growth factors (HGH, FGF-18, IGF1, TGF-β1) into biodegradable plastic (PLGA) microscopic spheres. These SASC were designed to release the growth factors slowly over the course of 28 days.
Arthritis is characterized by inflammation of cartilage at the joints. Cartilage is mostly made of collagen and chondrocytes, which are cells that secrete collagen. To model arthritis, the researchers grew chondrocytes in a dish and exposed them to inflammatory molecules commonly produced in arthritis patients. The “inflamed” chondrocytes were then treated with either normal (fat-derived) stem cells or SASC.
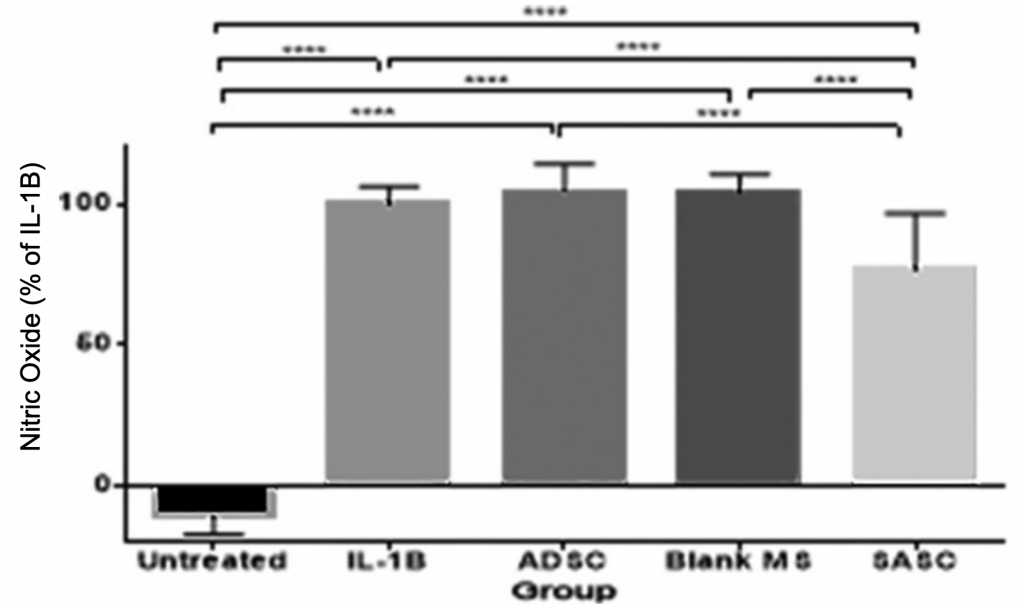
In arthritis patients, nitric oxide (NO) is activated by chondrocytes and is an indicator of inflammation. Thus, to assess inflammation in their cell model for arthritis, the researchers measured NO production. They found that while stem cell treatment did not reduce NO production, SASC treatment did, indicating the anti-inflammatory property of SASC.
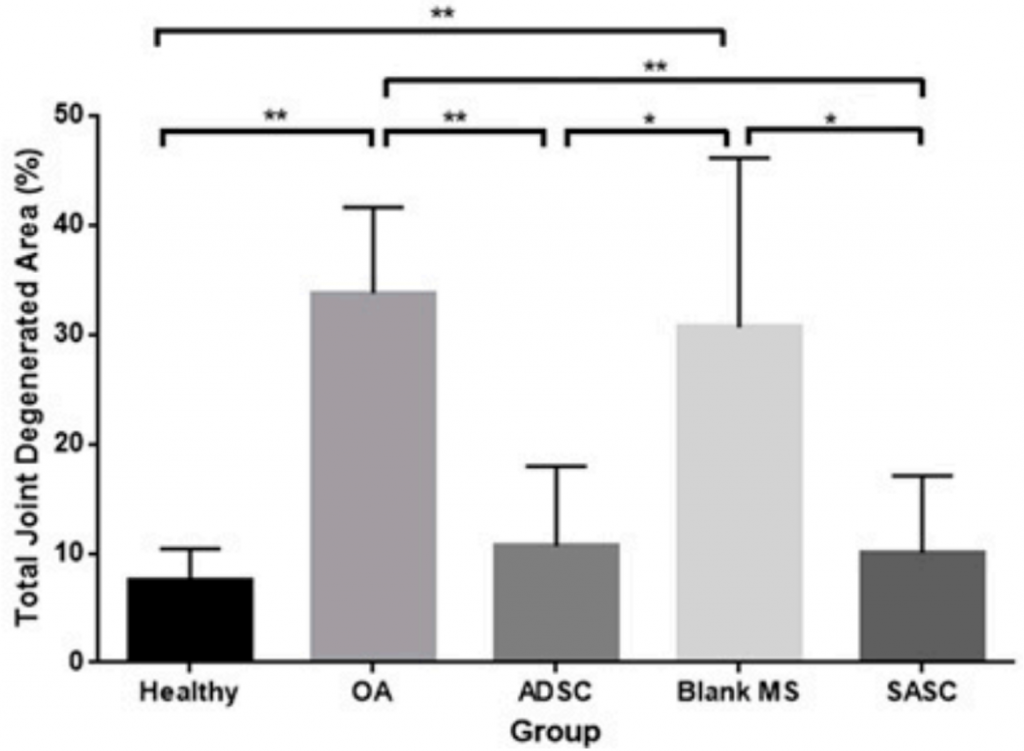
Arthritis is a degenerative disease caused by progressive wear and tear of cartilage at the joints. To determine if SASC can reduce cartilage degeneration, Shah and colleagues injected rats in the knee with an enzyme that breaks down collagen to model arthritis. They next injected stem cells or SASC particles as a treatment. A special dye was used to assess degenerated cartilage, and it was found that both stem cell and SASC-treated rats had degeneration comparable to healthy rats, indicating that both living stem cells and SASC can treat joint degeneration.
Can Artificial Stem Cells Treat Multiple Age-Related Diseases?
Depending on the tissue, the secretions of stem cells, deemed the secretome, can contain a range of molecules. For example, bone stem cells have been shown to secrete a protein called GDF-11, which alleviates muscle decline. While single factors like GDF-11 may be beneficial, the allure of SASC is that they can potentially be tailored to the needs of any organ with different combinations of factors. Furthermore, SASC could bypass the immune system rejection, tumor formation, and infections associated with living stem cells. Another advantage of SASC is that they have a longer shelf life, wider availability, and more scalability.
Clearly more studies are needed, as the work of Shah and colleagues is pioneering. However, with what we know, it seems feasible that SASC can be used to treat multiple degenerative diseases, which encompasses many age-related diseases, including sarcopenia (muscle degeneration) and neurodegeneration. Of course, cartilage is one of the simplest tissues, functioning mainly as a lifeless cushion. More complex tissues, such as brain tissue may be more difficult to regenerate while maintaining or restoring functions like memory. Still, treating arthritis and sarcopenia is definitely not trivial.