Key Points:
- Supplementing with rapamycin increases the rate at which the left ventricular heart chamber fills with oxygenated blood.
- Rapamycin supplementation increases the amount of blood left in the left ventricular chamber after contraction.
- Rapamycin increases blood vessel dilation after eight weeks of supplementation.
In a small pilot study, six males in their seventies took 1 mg of rapamycin for eight weeks. While none had active heart disease, five were on statins (drugs that lower cholesterol to reduce the risk of heart disease). Ultimately, rapamycin treatment improved certain aspects of the participants’ heart and blood vessel function, suggesting this longevity drug could potentially counteract cardiovascular aging.
Rapamycin’s Effect on the Heart
To assess the participants’ hearts, researchers from the Barshop Institute in Texas employed magnetic resonance imaging (MRI). MRI machines utilize a powerful electromagnetic field to generate detailed images of a target organ, such as the heart. Amazingly, blood flow within the heart can be measured using MRI, allowing researchers to measure how well the heart is pumping blood, its primary function.
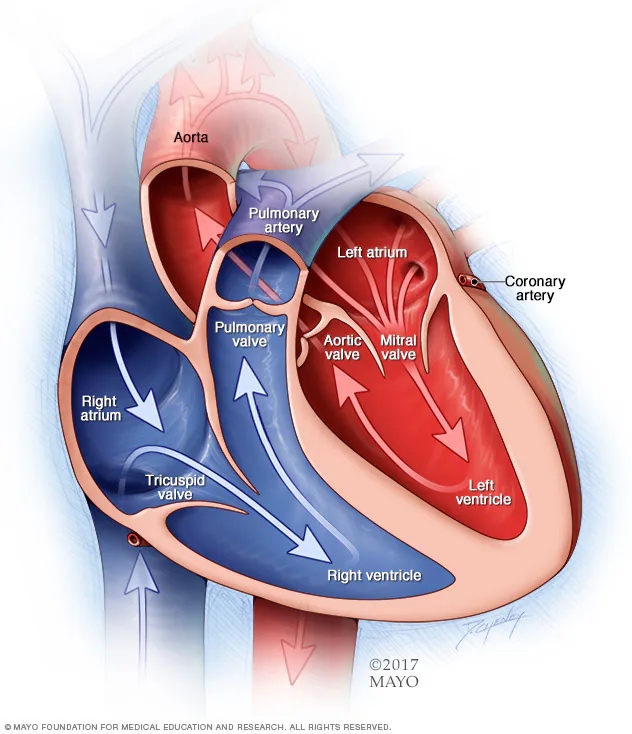
The heart is made up of four chambers: two atria, which receive blood, and two ventricles, which pump blood. While the right atrium and ventricle deal with deoxygenated blood, the left side of the heart deals with oxygenated blood. It follows that the left ventricle is responsible for pumping oxygenated blood to the entire body. The left ventricle is also the most vulnerable to aging, as its musculature stiffens with age.
When too stiff, the left ventricle is unable to stretch enough to accommodate normal volumes of blood. However, the researchers found that the filling rate of the left ventricle was increased in response to rapamycin treatment, suggesting the treatment reduces left-ventricle stiffness. Moreover, rapamycin increased the speed and volume of blood flowing through the mitral valve (from the left atrium to the left ventricle).
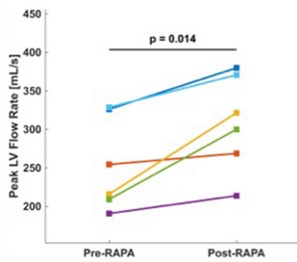
When the left ventricle contracts, some, but not all, of the blood within the chamber is pumped to the rest of the body. The remaining volume of blood within the left ventricle after contraction is called the end-systolic volume. The researchers found that rapamycin treatment increased the end-systolic volume. Curiously, this suggests that the left ventricle is not pumping as much blood as it was before rapamycin treatment.
A reduction in the blood-pumping capabilities of the left ventricle can be interpreted as the musculature of the left ventricle becoming weaker. This is somewhat in line with a previous study of heart transplant patients. In response to a heart transplant, the left ventricle hypertrophies (becomes larger). The transplant study showed that rapamycin reduces left ventricular hypertrophy. Thus, rapamycin may play a role in weakening the left ventricle in older men, suggesting further examination is needed.
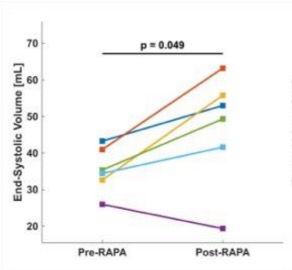
Ultimately, rapamycin treatment did not significantly alter cardiac output, which is the volume of blood the heart pumps per minute. It is unclear whether cardiac output, which decreases with age, would have declined over the eight-week trial period had the participants not been taking rapamycin. If cardiac output normally declines within eight weeks for older men, then rapamycin may prevent this. However, this will need to be addressed in a placebo-controlled clinical trial.
Rapamycin’s Effect on the Vasculature
Like the left ventricle of the heart, our blood vessels also stiffen with age. Our blood vessels, including our arteries and veins, have the capacity to stretch and dilate to accommodate a higher volume of blood, which increases blood flow. However, if our blood vessels, particularly our arteries, become stiff, we are more likely to suffer from a heart attack or a stroke.
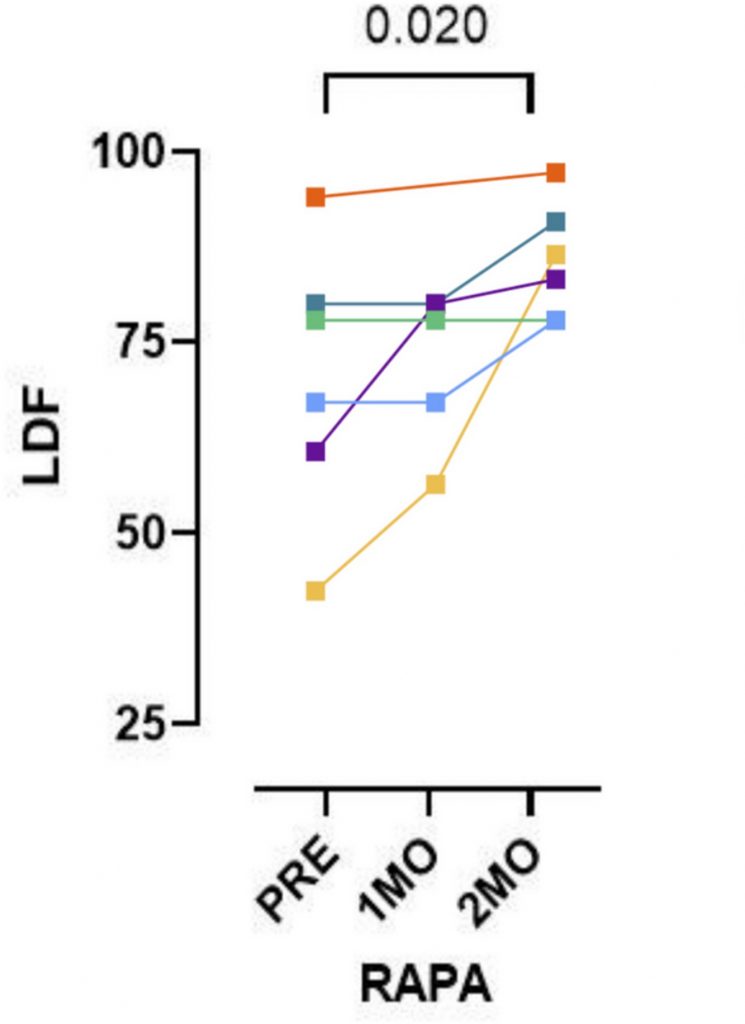
To assess blood vessel dilation, the researchers utilized technology called laser Doppler flowmetry (LDF). LDF is an optical technique that measures blood flow by analyzing the light reflected off red blood cells. To trigger blood vessel dilation, the researchers exploited the natural tendency of blood vessels to relax in response to heat (local thermal hyperemia). Namely, the researchers used LDF after applying heat to the forearms of the participants.
Due to events unrelated to the study, one of the participants could not complete the LDF experiment. Still, the results showed an increase in blood flow after eight weeks of rapamycin treatment in all five remaining participants. These findings suggest that rapamycin treatment counteracts blood vessel stiffening, one of the most dangerous symptoms of vascular aging. It follows that rapamycin could potentially reduce the risk of cardiovascular-related death.
Inhibiting mTOR for Healthy Aging
Rapamycin was originally approved by the Federal Drug Administration (FDA) to mitigate organ transplant rejection. Since then, it has been shown to prolong the lifespan of model organisms, including mice, to a similar degree as consuming fewer calories. Also in animal models, rapamycin has been shown to improve age-related deficits in brain, immune system, and heart function. These studies suggest that the pro-longevity effects of rapamycin primarily stem from the inhibition of the nutrient sensor mTOR (mechanistic target of rapamycin).
Known as rapalogs, there are multiple mTOR inhibitors on the market, including second-generation mTOR inhibitors like everolimus, which has fewer side effects than first-generation mTOR inhibitors like rapamycin (sirolimus). Considering its promise as a longevity intervention in animal studies, rapamycin has been tested in older adults in multiple clinical trials. However, the evidence gathered from human studies does not capture the profound effects seen in animal studies.
Still, the Barshop Institute study is promising, and mirrors some of the results from mouse studies. Larger studies with more participants and a placebo group may reveal that rapamycin plays a preventive role in age-related heart decline.